|
Aerobic Fitness Prevents Coronary Artery Disease
Author:
Stan Reents, PharmD
Original Posting:
09/13/2018 05:53 AM
Last Revision: 05/15/2019 08:51 AM
Deaths due to a coronary event occur at a rate of approximately one every minute in the US! As such, coronary artery disease deserves more attention than it gets.
Even worse than the huge number of people dying from coronary disease every year is that researchers have estimated that 80-90% of heart disease can be prevented (Kones R. 2011) (Mozaffarian D, et al. 2008). Risk factors for coronary artery disease include: elevated blood pressure, elevated blood lipids, smoking, diabetes, obesity, stress, family history of heart disease, and, most importantly, lack of exercise, specifically, aerobic exercise. Other than "family history," each of these risk factors can be modified with lifestyle changes.
In my opinion, nothing -- absolutely NOTHING -- is more effective for coronary artery disease than aerobic exercise.
Now it's certainly not news to state that exercise is good for your heart. But what I will explain here is how effective maintaining your aerobic fitness can be. (NOTE: This review is a companion to Exercise for Coronary Artery Disease.)
But first:
Coronary artery disease is a serious medical condition! While exercise is clearly one of the best things you can do, talk to your personal physician before you decide to embark on a new exercise program. Then, once you receive the go-ahead, use this article to guide you.
CURRENT AEROBIC EXERCISE RECOMMENDATIONS: Official Guidelines
Current exercise recommendations for otherwise healthy adults are to perform moderate intensity aerobic exercise 150 minutes per week. An example of "moderate intensity" aerobic exercise is brisk walking.
But this is just a general recommendation to maintain your health. Is this amount of exercise enough to prevent coronary artery disease?
Yes, it can be for most people. In 2011, public health experts from Harvard, Stanford, and the University of Texas reviewed 33 published research studies and concluded the following (Sattelmair J, et al. 2011):
AMOUNT OF
"MODERATE" INTENSITY
EXERCISE
PER WEEK |
PERCENT REDUCTION
IN RISK OF
CORONARY ARTERY DISEASE |
| • 150 minutes/week |
14% reduction |
| • 300 minutes/week |
20% reduction |
So, 150 min/week (ie., 30 min/day, 5 days/week) is acceptable, but 300 min/week is better.
If your aerobic exercise sessions are vigorous, then, you don't have to exercise as long. The American College of Sports Medicine (ACSM) has recognized this principle for years in their official exercise recommendations: if vigorous aerobic exercise is performed, then a 20-minute session 3 times per week is enough.
It turns out that how "hard" your aerobic exercise sessions are is probably more important than how "long" they are. I'll discuss this concept further down....
WHAT TYPE OF EXERCISE IS BEST FOR CORONARY ARTERY DISEASE?
For preventing and reversing coronary artery disease, aerobic types of exercise are best: walking, hiking, jogging, biking, swimming, basketball, tennis, soccer, etc.
On November 12, 2013, the American College of Cardiology (ACC) and the American Heart Association (AHA) published their latest "Guidelines for Lifestyle Management to Reduce Cardiovascular Risk" (Eckel RH, et al. 2013). In this report, they recommend that people who have an elevated cholesterol level and/or elevated blood pressure perform aerobic exercise 40 min/day, on 3-4 days/week. In formulating this "official" recommendation, the ACC and AHA committees included the findings from Harvard/Stanford/U. Texas research.
What about other types of exercise?
Aerobic Exercise: "Duration" vs. "Intensity"
A large Harvard study of male health care professionals shows how effective various types of exercise are in lowering the risk of coronary disease (Tanasescu M, et al. 2002):
| TYPE OF EXERCISE |
AMOUNT |
REDUCTION IN RISK
OF
CORONARY ARTERY DISEASE |
| • Running |
1 hr
per WEEK
or more |
42% reduction |
| • Weight-training |
30 min
per WEEK
or more |
23% reduction |
| • Rowing |
1 hr
per WEEK
or more |
18% reduction |
| • Brisk walking |
30 min
per DAY
or more |
18% reduction |
In the table above, note how much more effective running is compared to walking....even though running was only performed 1 hour per week! (ie., this would be equivalent to the ACSM recommendation of 20 minutes/day, 3 days per week). In other words, to decide if a particular activity is beneficial, duration and intensity both need to be considered.
HEALTHY CORONARY ARTERIES IN RUNNERS
Except for ultra-endurance exercise, running is clearly good for your coronary arteries. Described below are 2 famous examples:
Clarence DeMar: Olympic Marathon Runner
Clarence DeMar was a well-known marathon runner. He ran competitively from age 21 until age 69. He was a 7-time winner of the Boston Marathon and a member of 3 Olympic teams.
In 1961, his autopsy results were published in the New England Journal of Medicine. (Paul Dudley White, MD, the Boston cardiologist who consulted on President Eisenhower when he suffered a heart attack in 1955, was an author of this paper.) It was revealed that Mr. DeMar's coronary arteries were 2-3 times larger than normal (Currens JH, et al. 1961).
Now, admittedly, this doesn't prove that marathon running was the reason for his larger coronary arteries, but it sure is darn likely! Unfortunately, we don't know anything about his diet and we don't know what his measured VO2max value was. But we do know that Mr. DeMar didn't die from heart disease. He died of cancer at age 70.
Nathan Pritikin: Founder of The Pritikin Longevity Center
There is no more dramatic example of the power of lifestyle changes to reverse coronary artery disease than the case of Nathan Pritikin:
In December 1955, Mr. Pritikin had a total cholesterol level of 280 mg/dL (LDL and HDL fractions were not done back then). At that time, he began to modify his diet.
In February 1958, he was diagnosed with asymptomatic coronary insufficiency (ie., inadequate blood flow through the coronaries without producing symptoms of chest pain). At this point, he became much more disciplined about his diet by restricting his consumption of fat and cholesterol. And, he began running. The impact of these changes on his total cholesterol levels are summarized in the table below:
| DATE |
TOTAL
CHOLESTEROL |
| Dec. 1955 |
280 mg/dL |
| Feb. 1958 |
210 mg/dL |
| July 1958 |
162 mg/dL |
| Sept. 1958 |
122 mg/dL |
| Aug. 1959 |
155 mg/dL |
| June 1960 |
120 mg/dL |
| Dec. 1963 |
102 mg/dL |
| March 1966 |
119 mg/dL |
| Sept. 1968 |
118 mg/dL |
| Jan. 1969 |
112 mg/dL |
| Nov. 1984 |
94 mg/dL |
Mr. Pritikin lived for another 27 years after his diagnosis of coronary insufficiency. He died in 1985, at the age of 69. The cause of death was "complications" from lymphoma, not heart disease.
Even more remarkable than the fact that he kept his (total) cholesterol at 120 mg/dL or lower for 25 years is what was discovered during his autopsy: when his coronary arteries were opened, there were no raised plaques and there was no constriction of the lumen (the inside diameter of the arteries). Whereas he initially had serious coronary atherosclerosis, he had completely reversed it with only diet and aerobic exercise! This case was also published in the New England Journal of Medicine (Hubbard JD, et al. 1985).
Mr. Pritikin figured out how to reverse his coronary disease with only lifestyle changes nearly 60 years ago! But keep in mind that he made 2 improvements in his lifestyle: (a) he changed his diet (drastically!) and (b) he substantially improved his aerobic fitness. Unfortunately, here again we don't know what his actual aerobic fitness level (VO2max) was.
Aerobic Exercise: High-Intensity Interval Training
More recently, the concept of including short bursts of high-intensity effort into an aerobic exercise session has become popular. Exercise professionals call this "high-intensity training" (HIT) or "high-intensity interval training" (HIIT). This type of exercise session improves your aerobic capacity (VO2max).
A study from McMaster University in Canada published in Medicine and Science in Sports and Exercise showed that very short bursts of higher-intensity aerobic exercise were also effective in coronary artery disease:
• Patients with documented CAD were randomized to 2 different exercise programs: One group rode a stationary bike for 1-min at an intense pace, followed by 1-min of rest. This was repeated for a total of 10 intervals. The other group rode at a more moderate intensity for 50 minutes/session. Exercise sessions were conducted twice per week for 12 weeks. The 20-minute sessions of high-intensity, short bursts were just as effective in improving vascular function and aerobic fitness levels as the 50 minute sessions (Currie KD, et al. 2013).
**WARNING**: If you have heart disease, you should not attempt any kind of intense exercise without first receiving medical clearance from your personal physician. And, even then, increase the intensity of your exercise sessions gradually.....ie., walk briskly for 2-4 weeks first, then consider increasing the intensity. At all times, it is wise to monitor your HR during your exercise session. Stop exercising immediately if you develop chest pain or pressure, pain radiating to your shoulder or down your arm, or, the sensation that you can't catch your breath.
MAINTAINING AEROBIC FITNESS REDUCES CORONARY ARTERY DISEASE RISK MORE THAN ANY OTHER LIFESTYLE BEHAVIOR
Numerous clinical studies published over the span of several decades show that a poor aerobic fitness level (VO2max) is an independent risk factor for heart disease. This has been documented in men (Balady GJ, et al. 2004) (Lauer MS, et al. 1996) and in women (Gulati M, et al. 2003) (Mora S, et al. 2003).
Steven Blair, PED, a researcher at the University of South Carolina, analyzed data from over 50,000 patients studied at the Cooper Institute. He calculated how much each risk factor contributed to death in these patients. He concluded that "poor aerobic fitness level" is a greater contributor to the risk of cardiovascular death than are any of the traditional risk factors that clinical medicine currently monitors, eg., cholesterol levels, presence of diabetes or obesity, and even smoking. He found that poor aerobic fitness accounted for 16-17% of deaths whereas high cholesterol levels were responsible for only 2-4% (Blair SN. 2009). (In the graph below, aerobic fitness level is identified as "CRF": cardiorespiratory fitness.) 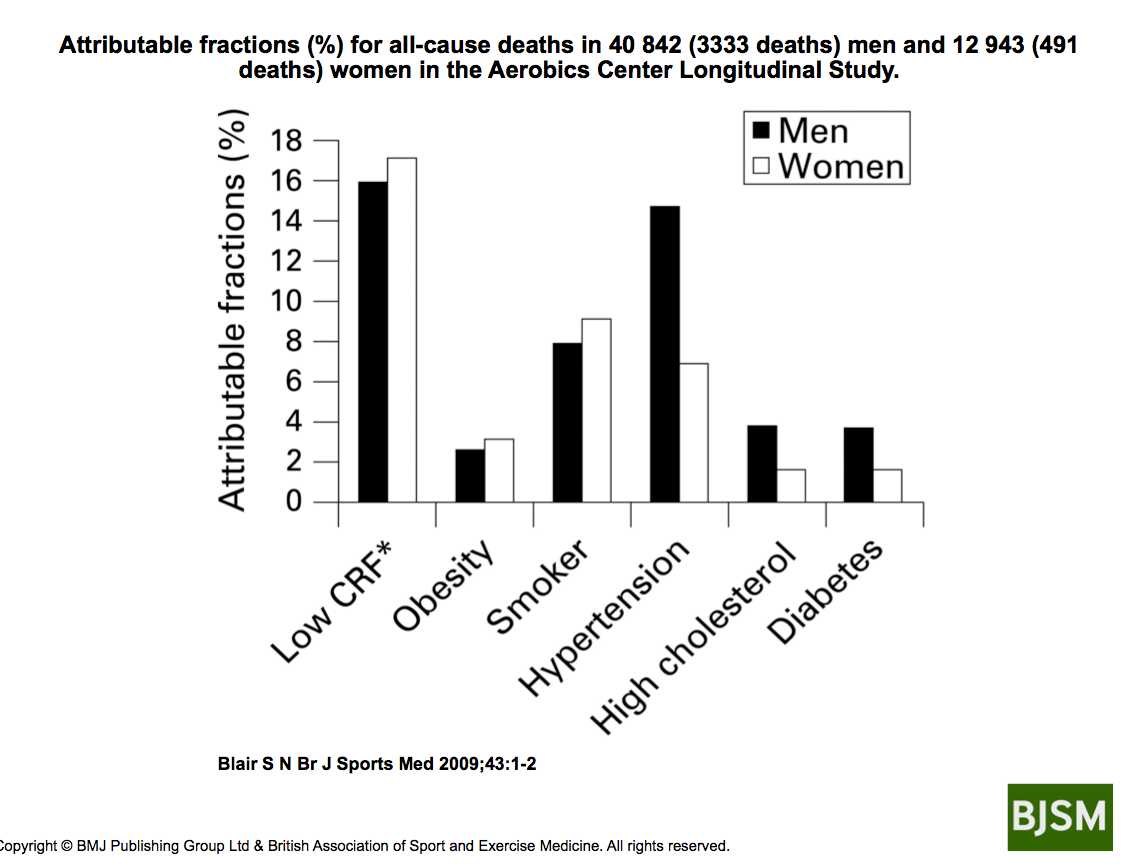
As discussed above, aerobic fitness (VO2max) can be improved by running, or, by doing some short, high-intensity bursts. Regardless of how it is achieved, aerobic fitness is highly beneficial for coronary artery disease:
• In 1998, researchers at the Cooper Institute reported that cardiovascular mortality decreased as aerobic fitness increased in 25,000 men. This trend held true regardless of their cholesterol level (Farrell SW, et al. 1998).
• In November 2012, a subsequent study from the Cooper Institute was published in Medicine and Science in Sports and Exercise. Nearly 41,000 men were monitored for an average of 17 years. The investigators found that high degrees of aerobic fitness substantially reduced the risk of death from coronary artery disease regardless of what a person's LDL-cholesterol level was. In fact, a person with an LDL-cholesterol of < 100 mg/dL but with a poor degree of aerobic fitness had a greater risk than a person with a very high LDL level of > 190 mg/dL and excellent aerobic fitness (Farrell SW, et al. 2012)!
CALCULATING HEART DISEASE RISK: THE "RISK FACTOR GAP"
Why is maintaining your aerobic fitness so effective at preventing coronary disease?
I've explained the hemodynamic and metabolic effects of exercise in detail in the companion review Exercise and Coronary Artery Disease. But, the short answer is because aerobic exercise improves dozens of physiologic functions simultaneously.
Recently, a "risk factor gap" has been identified when evaluating a person's risk for a heart attack (myocardial infarction). It turns out that relying on traditional health/disease markers such as cholesterol levels, blood pressure, etc. don't tell the whole story.
• Researchers from Harvard monitored over 27,000 healthy women for an average of 11 years. They concluded that only 59% of the benefit of exercise (in reducing risk) could be explained by improvements in traditional risk factors....ie., a reduction in blood pressure, improvement in cholesterol, decreased insulin resistance, etc (Mora S, et al. 2007).
Thus, in addition to its ability to improve "traditional" risk factors, this means that as much as 41% of the benefit of exercise is due to a direct effect, a very impressive level of impact!
In other words, not only does exercise improve multiple risk factors simultaneously, but, also, exercise produces direct effects on coronary arteries, on various components of the blood, and provides numerous other beneficial actions. To achieve the same results with drug therapy would require 4 or 5 or 6 drugs. And, even then, you still wouldn't get all the health benefits that aerobic exercise provides!
The American Heart Association had identified this "risk factor gap" phenomenon in an official white paper on the prevention of atherosclerotic cardiovascular disease published in 2003 (Thompson PD, et al. 2003). In it, they stated:
"In many studies, the lower frequency of CAD [in more physically active people] was independent of other known atherosclerotic risk factors."
Aerobic Fitness Should be Part of the Risk Calculation Equation
And, including specific measurements of aerobic fitness can dramatically improve the accuracy of common heart disease risk scoring systems such as the Framingham Risk Score (FRS) and the European risk scoring system "SCORE":
• A 2011 evaluation based on more than 66,000 patients studied at the Cooper Institute ("Cooper Center Longitudinal Study") reported that, when a test of fitness level was added to the European risk scoring system, which evaluates risk for death due to cardiovascular disease, over 10% of the subjects required reclassification (Gupta S, et al. 2011).
• When assessments of fitness level were incorporated into the widely-known Framingham Risk Score (FRS), in one study, nearly half of the subjects had to be reclassified from low or intermediate risk to high risk (Mora S, et al. 2005). Similar studies in women also showed that fitness assessments greatly enhanced the accuracy of the Framingham Risk Score (Gulati M, et al. 2003) (Mora S, et al. 2003).
It now appears that aerobic fitness is far more critical in determining your risk of a heart attack than are any of the other risk factors regularly monitored.
Here is a statement from researchers conducting the Cooper Center Longitudinal Study (CCLS) that provides a perspective on how risk of death decreases as fitness level improves:
"A 55-year old man who requires 15 minutes to walk 1 mile is considered to have a low level of fitness. We would predict that his lifetime risk for death due to cardiovascular disease is nearly 30%. In contrast, a man able to run a mile in 10 minutes has a moderate degree of fitness and has an estimated lifetime risk of CVD mortality of just 10%." (Berry JD, et al. 2011).
Thus, gauging the risk for coronary heart disease can be very misleading if the impact of exercise (aerobic fitness) is ignored. Poor aerobic fitness also helps to explain why heart disease can progress despite reducing the LDL-cholesterol value to very low levels with drug therapy.
It is my opinion that these earlier determinations of heart disease risk based on cholesterol levels are flawed because they excluded "exercise" (or, even better, measurements of aerobic fitness) from the analysis...ie., a "risk factor gap" exists if aerobic fitness is not assessed.
PERSPECTIVE
In 1992 (finally!), the American Heart Association first recognized that "physical inactivity" was a major risk factor for coronary artery disease. However, 24 years passed before they published their Scientific Statement "Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign" in the December 13, 2016 issue of Circulation (Ross R, et al. 2016.)
Why has it taken the medical profession so long to embrace exercise as a highly effective therapy for coronary artery disease?
1) Regular aerobic exercise is the best thing you can do to prevent coronary artery disease.
Although all risk factors for coronary artery disease should be addressed, I now believe that an improvement in aerobic fitness is the most important.
Aerobic exercise is powerful and offers numerous benefits. It improves multiple "traditional" risk factors simultaneously...ie., it can lower blood pressure, improve insulin resistance, lead to weight loss, improve blood lipids, and reduce stress. But, in addition, aerobic exercise provides other physiologic benefits on the cardiovascular system. These include an enhanced ability of the coronary arteries to dilate (expand) on demand, a slower resting HR, favorable changes in other blood components, etc. To achieve the same results with drug therapy, you would have to take several drugs, and even then, you still wouldn't obtain all of the benefits that regular aerobic exercise provides.
In study after study, aerobic exercise (in the right amount and at the right intensity) has been shown to reduce coronary "events" and reduce death from cardiovascular disease. And this occurs even if: cholesterol levels don't change, no weight is lost, and no dietary changes are made.
It is clear that aerobic exercise yields the most "bang for the buck" in the management of coronary artery disease.
2) Estimations of heart disease risk must include a measurement of aerobic fitness to be accurate.
There is an uncomfortable discrepancy between research showing that lowering LDL-cholesterol reduces the risk of coronary artery disease, and other research showing a high rate of heart attacks even when patients have so-called "desirable" cholesterol levels. This suggests that risk estimations are unreliable. Even the widely-recognized Framingham Risk Score (FRS) and the European risk score "SCORE" have been shown to provide misleading estimations: when an assessment of aerobic fitness was added into the equation, the risk estimation was substantially different. Epidemiologist Steven Blair, PED, has determined that a poor degree of aerobic fitness is 16-17% responsible for deaths due to cardiovascular disease, whereas an elevated cholesterol level is only 2-4% responsible (Blair SN. 2009).
Thus, I believe that the numerous studies that attempt to relate the risk of coronary disease to the LDL-cholesterol blood test are flawed if they have not included activity level (fitness level) in the analysis (the "risk factor gap"). In any event, the following cannot be denied:
(a) even when LDL-cholesterol levels are in the "acceptable" range, a disturbingly high percentage of people still have heart attacks
(b) regular aerobic exercise reduces the rate of coronary events regardless of the LDL-cholesterol level
In other words, a high degree of aerobic fitness can offset the risks of a high LDL-cholesterol level. However, a low LDL-cholesterol level cannot offset a poor degree of aerobic fitness (Farrell SW, et al. 2012).
3) Coronary artery disease is not a disease.....it's an "Exercise Deficit!"
I now believe that it is better to think of coronary artery disease (indeed, ALL clinical manifestations of atherosclerosis!) as an "exercise deficit" more than as a "disease" in the classic sense.
In my opinion, a health problem that can be so easily induced and reversed by changes in exercise level does not meet my definition of a "disease"...certainly not like conditions such as cystic fibrosis, leukemia, lupus, schizophrenia, sickle cell disease, etc. Diseases like these cannot be induced and reversed by lifestyle changes.
Instead, in the majority of patients, coronary artery disease is more like conditions such as dandruff, athlete's foot, and tooth decay. These conditions are not really "diseases"....rather, they simply reflect an improper health "behavior."
Assuming the estimate that 80-90% of cases of heart disease are preventable is accurate, then, I think the medical profession (and society in general) needs to devote much more effort to prevention of this health problem. The medical profession should shift its perspective on coronary artery disease (and other manifestations of atherosclerosis) from regarding it as a genetic disorder, or, a biochemical disease, and begin thinking of it as an "exercise deficit." Exercise should not be thought of as something that patients should "also" do but, rather, something that they must do. We can realize better results and spend fewer health care dollars by intensifying our message that exercise is good for everyone and less on trying to find the one genetic deficit, or, the one molecule in the bloodstream that causes coronary artery disease.
Realtors often say that the 3 most important factors when evaluating a house to buy are "location, location, and location." Similarly, I propose that the 3 most important factors for preventing coronary heart disease are:
1) aerobic exercise
2) aerobic exercise
3) aerobic exercise
I believe once we think of coronary artery disease in terms of replacing the missing ingredient -- aerobic exercise -- and not only focusing on lowering LDL-cholesterol, we will do a better job of reducing morbidity and mortality.
A lot of research was reviewed. Here are the critical points:
"STEPS" YOU SHOULD TAKE: 1) Perform Aerobic Exercise Regularly
• For otherwise healthy adults: Current official exercise guidelines for otherwise healthy adults say that you should shoot for 150 minutes per week of "moderate intensity" aerobic exercise. An example of how to meet this target is brisk walking for 30 minutes per day 5-7 days per week. After you have been exercising at a moderate intensity level for several weeks, if you wish to save time, consider doing short bursts of higher-intensity exercise. Monitoring your HR while you exercise is strongly recommended. Consider wearing a HR monitor. Resistance exercise is also beneficial, but, aerobic exercise is better (Thompson PD, et al. 2003).
• If you already have an elevated cholesterol and/or elevated blood pressure: The latest guidelines from the American College of Cardiology and the American Heart Association recommend 40 minutes of aerobic exercise per day, on 3-4 days per week. (Eckel RH, et al. 2013).
"STEPS" YOU SHOULD TAKE: 2) Monitor Your Aerobic Fitness
Let's say you've been exercising regularly. How do you know if you've improved your aerobic fitness?
Blood flow (oxygen delivery) is the critical variable in coronary artery disease. It is assessed with several tests:
Exercise EKG
For decades, cardiologists have evaluated coronary blood flow (oxygen delivery) with a test called the "exercise EKG." During this test, the patient walks or runs on a treadmill, or rides a stationary bicycle, while being monitored with an EKG. Poor blood flow through the coronary arteries shows up on the EKG tracing. However, measurements of exercise capacity and how quickly your heart rate decreases right after exercise stops ("heart rate recovery") are better predictors of risk (Greenland P, et al. 2010).
VO2max
The most accurate way to assess your aerobic fitness is by measuring your "VO2max". This test is most often performed by running on a treadmill. During this test, you are breathing through a snorkel and you must run hard. It can also be done on an exercise bike or a rowing machine.
The highest VO2max value ever recorded was in elite cross-country skier Bjorn Daehlie. The values for cyclist Greg Lemond (he won the Tour de France 3 times) and middle-distance runner Steve Prefontaine are also listed in the table below.
The values in these world-class athletes contrast with the very low values documented in patients with heart disease (Ades PA, et al. 2006). People with a VO2max value below 20 ml/kg/min have such poor aerobic fitness that they can't run even a single lap around a high-school track:
| WHO? |
VO2max |
| • Bjorn Daehlie (cross-country skier) |
94 ml/kg/min |
| • Greg Lemond (cyclist) |
92-94 ml/kg/min |
• Steve Prefontaine
(middle-distance runner) |
84 ml/kg/min |
| • Cardiac Rehab Patients: males |
19 ml/kg/min |
| • Cardiac Rehab Patients: females |
14 ml/kg/min |
While VO2max is one of the most important physiologic parameters to know, measuring it like I have described above is complicated, costs time and money, and, just doesn't qualify as a simple screening test....which is what people need.
It turns out you can assess your aerobic fitness (and the health of your vascular system) without the need for a complicated medical or laboratory test:
Resting Heart Rate
Numerous research studies show that, as your aerobic fitness improves, your resting HR will slow down. This is good!
So, resting HR mimics your level of aerobic fitness. But, does it provide an indication of your vascular health?
Yes, according to Paolo Palatini, MD: "More than 50 articles have been published on the significance of elevated HR......all but 2 reported an association between fast HR and all-cause mortality in men." (Palatini P, 2009). (the first study to focus attention on this was published in 1945!) Here are several examples:
• Over 5700 men in France were followed for 23 years. It was found that men with a resting HR of 75 or higher had a 3.5-fold increased risk of sudden death compared to men with a resting HR of 60 or less (Jouven X, et al. 2005).
• Men and women in Norway who had a resting HR of 70 or lower during their first assessment, but, had a resting HR of 85 or higher 12 years later, had a nearly 2-fold increased risk of death from coronary artery disease (Nauman J, et al. 2011).
• In April 2013, researchers from Denmark evaluated nearly 3000 men with no history of cardiovascular disease and monitored them for 16 years. They found that an elevated resting HR was an independent risk factor for death (Jensen MT, et al. 2013).
This means that your resting HR is something you should keep track of on a regular basis. Here's how to do it:
The best time to check your resting HR is right when you wake up.
- The night before: do not drink any alcohol; put a clock or watch next to your bed.
- As soon as you awake, before even sitting up, take your pulse. This can be done by placing 2 fingers on the side of your throat or on the back of your wrist.
- Count your pulse for 15 seconds and multiply by 4.
- Goal: a resting HR of 70 bpm or less.
Measure your resting HR once or twice per month.
We're big fans of wearing a heart rate monitor while exercising. We list some good ones here: Heart Rate Monitors.
For more information on how you can use your heart rate to monitor your health and fitness, see: "Heart Rate, Exercise Intensity, and Training".
Resting HR is a simple but very sensitive indicators of vascular "function" that you can monitor. Every minute of every day, your heart rate is a reflection of oxygen delivery. And erectile function in men is useful because this can develop years before symptoms of angina appear. This is because the arteries responsible for erection are much smaller in diameter than the arteries in the heart that must fail for chest pain to occur.
DISCLAIMER: Readers should keep in mind that, while there is ample scientific research supporting the logic of using resting HR to assess vascular function, these parameters have not been included in widely-accepted risk screening calculations such as Framingham (USA), SCORE (UK), etc (Greenland P, et al. 2010) nor have they been endorsed by "official" treatment guidelines, such as those from the American Heart Association/American College of Physicians (Qaseem A, et al. 2012). However, the research summarized above does suggest that these simple physiologic indicators can be highly useful in assessing the health of your vascular system. Also, the most recent (August 2013) AHA guidelines for exercise testing do endorse "recovery" heart rate as a valuable parameter to use (Fletcher GF, et al. 2013).
CONCLUSION
Don't wait for your physician to tell you that you need to start exercising, and definitely don't get so out-of-shape that you begin having symptoms like chest pain. Do some form of aerobic exercise several times per week.
And now that you've finished reading this review, shut off your computer and go for a brisk run!
FOR MORE INFORMATION
Readers may also be interested in:
EXPERT HEALTH and FITNESS COACHING
Stan Reents, PharmD, is available to speak on this and many other exercise-related topics. (Here is a downloadable recording of one of his Health Talks.) He also provides a one-on-one Health Coaching Service. Contact him through the Contact Us page.
REFERENCES
Ades PA, Savage PD, Brawner CA, et al. Aerobic capacity in patients entering cardiac rehabilitation. Circulation 2006;113:2706-2712. Abstract
Balady GJ, Larson MG, Vasan RS, et al. Usefulness of exercise testing in the prediction of coronary disease risk among asymptomatic persons as a function of the Framingham Risk Score. Circulation 2004;110:1920-1925. Abstract
Belardinelli R, Paolini I, Cianci G, et al. Exercise training intervention after coronary angioplasty: The ETICA Trial. J Am Coll Cardiol 2001;37:1891-1900. Abstract
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics - 2018 update. Circulation 2018;137:e67-e492. Abstract
Berry JD, Willis B, Gupta S, et al. Lifetime risks for cardiovascular disease mortality by cardiorespiratory fitness levels measured at ages 45, 55, and 65 years in men: the Cooper Center Longitudinal Study. J Am Coll Cardiol 2011;57:1604-1610. Abstract
Blair SN. Physical inactivity: the biggest public health problem of the 21st century. Br J Sport Med 2009;43:1-2. Abstract ***RECOMMENDED READING FOR ALL PRIMARY CARE PHYSICIANS***
Currens JH, White PD. Half a century of running: clinical, physiologic and autopsy finding in the case of Clarence DeMar (Mr. Marathon). N Engl J Med 1961;265:988-993. Abstract
Currie KD, Dubberley JB, McKelvie RS, et al. Low-volume, high-intensity interval training in patients with CAD. Med Sci Sports Exercise 2013;45:1436-1442. Abstract
Dong JY, Zhang YH, Qin LQ. Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol 2011;58:1378-1385. Abstract
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol. The Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA 1998;279:1615-1622. Abstract
Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. Circulation 2014;129 (25 Suppl 2):S76-S99. Abstract
Farrell SW, Kampert JB, Kohl HW, et al. Influences of cardiorespiratory fitness levels and other predictors on cardiovascular disease mortality in men. Med Sci Sports Exerc 1998;30:899-905. Abstract
Farrell SW, Finley CE, Grundy SM. Cardiorespiratory fitness, LDL cholesterol, and CHD mortality in men. Med Sci Sports Exerc 2012;44:2132-2137. Abstract ***RECOMMENDED READING FOR ALL PRIMARY CARE PHYSICIANS***
Fletcher GF, Ades PA, Kligfield P, et al. Exercise standards for testing and training. A scientific statement from the American Heart Association. Circulation 2013;128:873-934. Abstract
Greenland P, Alpert JS, Beller GA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults. J Am Coll Cardiol 2010;56:e50-e103. Abstract
Gulati M, Pandey DK, Arnsdorf MR, et al. Exercise capacity and the risk of death in women. The St. James Women Take Heart Project. Circulation 2003;108:1554-1559. Abstract
Gupta S, Rohatgi A, Ayers CR, et al. Cardiorespiratory fitness and classification of risk of cardiovascular disease mortality. Circulation 2011;123:1377-1383. Abstract
Hamalainen H, Luurila OJ, Kallio V, et al. Long-term reduction in sudden deaths after a multifactorial intervention programme in patients with myocardial infarction: 10-year results of a controlled investigation. Eur Heart J 1989;10:55-62. Abstract
Hambrecht R, Walther C, Mobius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease. Circulation 2004;109:1371-1378. Abstract
Hedback B, Perk J, Wodlin P. Long-term reduction of cardiac mortality after myocardial infarction: 10-year results of a comprehensive rehabilitation programme. Eur Heart J 1993;14:831-835. Abstract
Hubbard JD, Inkeles S, Barnard RJ. Nathan Pritikin's heart. N Engl J Med 1985;313:52. Abstract
Hurst JW. Paul Dudley White: to know him better. Am J Cardiol 1985;56:169-177. Abstract
Jensen MT, Suadicani P, Hein HO, et al. Elevated resting heart rate, physical fitness and all-cause mortality: a 16-year follow-up in the Copenhagen Male Study. Heart 2013;99:882-887. Abstract
Jouven X, Empana J-P, Schwartz PJ, et al. Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med 2005;352:1951-1958. Abstract
Kones R. Primary prevention of coronary heart disease: integration of new data, evolving views, revised goals, and role of rosuvastatin in management. A comprehensive survey. Drug Design Devel Ther 2011;5:325-380. Abstract
Kramsch DM, Aspen AJ, Abramowitz BM, et al. Reduction of coronary atherosclerosis by moderate conditioning exercise in monkeys on an atherogenic diet. N Engl J Med 1981;305:1483-1489. Abstract
LaCroix AZ, Leveille SG, Hecht JA, et al. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? J Am Geriatr Soc 1996;44:113-120. Abstract
Lauer MS, Okin PM, Larson MG, et al. Impaired heart rate response to graded exercise. Prognostic implication of chronotropic incompetence in the Framingham Heart Study. Circulation 1996;93:1520-1526. Abstract
Montorsi F, Briganti A, Salonia A, et al. Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. Eur Urol 2003;44:360-365. Abstract
Mora S, Redberg RF, Cui Y, et al. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: a 20-year follow-up of the lipid research clinics prevalence study. JAMA 2003;290:1600-1607. Abstract
Mora S, Redberg RF, Sharrett AR, et al. Enhanced risk assessment in asymptomatic individuals with exercise testing and Framingham risk scores. Circulation 2005;112:1566-1572. Abstract
Mora S, Cook N, Buring JE, et al. Physical activity and reduced risk of cardiovascular events. Potential mediating mechanisms. Circulation 2007;116:2110-2118. Abstract
Mozaffarian D, Wilson PWF, Kannel WB. Beyond established and novel risk factors: Lifestyle risk factors for cardiovascular disease. Circulation 2008;117:3031-3038. Abstract
Nauman J, Janszky I, Vatten LJ, et al. Temporal changes in resting heart rate and death from ischemic heart disease. JAMA 2011;306:2579-2587. Abstract
Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998;280:2001-2007. Abstract
Palatini P. Elevated heart rate: a "new" cardiovascular risk factor? Prog Cardiovasc Dis 2009;52:1-5. Abstract
Pitt B, Mancini GB, Ellis SG, et al. Pravastatin limitation of atherosclerosis in the coronary arteries (PLAC i): Reduction in atherosclerosis progression and clinical events. J Am Coll Cardiol 1995;26:1133-1139. Abstract
Qaseem A, Fihn SD, Dallas P, et al. Management of stable ischemic heart disease: Summary of a clinical practice guideline from the American College of Physicians/American College of Cardiology Foundation/American Heart Association/American Association for Thoracic Surgery/Preventive Cardiovascular Nurses Association/Society of Thoracic Surgeons. Ann Intern Med 2012;157:735-743. Abstract
Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: A case for fitness as a clinical vital sign. Circulation 2016;134:e653-e699. Abstract ***RECOMMENDED READING FOR ALL PRIMARY CARE PHYSICIANS***
Sattelmair J, Pertman J, Ding EL, et al. Dose response between physical activity and risk of coronary heart disease. A meta-analysis. Circulation 2011;124:789-795. Abstract
Tanasescu M, Leitzmann MF, Rimm EB, et al. Exercise type and intensity in relation to coronary heart disease in men. JAMA 2002;288:1994-2000. Abstract
Thompson PD, Buchner D, Pina IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease. Circulation 2003;107:3109-3116. Abstract
Vlachopoulos CV, Terentes-Printzios DG, Ioakeimidis NK, et al. Prediction of cardiovascular events and all-cause mortality with erectile dysfunction: a systematic review and meta-analysis of cohort studies. Circ Cardiovasc Qual Outcomes 2013;6:99-109. Abstract
Walther C, Mobius-Winkler S, Linke A, et al. Regular exercise training compared with percutaneous intervention leads to a reduction of inflammatory markers and cardiovascular events in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil 2008;15:107-112. Abstract
ABOUT THE AUTHOR

Stan Reents, PharmD, is a former healthcare professional. He is a member of the American College of Lifestyle Medicine (ACLM) and a member of the American College of Sports Medicine (ACSM). In the past, he has been certified as a Health Fitness Specialist by ACSM, as a Certified Health Coach by ACE, as a Personal Trainer by ACE, and as a tennis coach by USTA. He is the author of Sport and Exercise Pharmacology (published by Human Kinetics) and has written for Runner's World magazine, Senior Softball USA, Training and Conditioning and other fitness publications.
Browse By Topic:
aerobic exercise, coronary artery disease, exercise and health, exercise guidelines, exercise information, exercise motivation, exercise recommendations, health and fitness targets, heart disease, measuring fitness
Copyright ©2026 AthleteInMe,
LLC. All rights reserved.
|